What Is Dermatillomania? Causes, Symptoms, and Treatment
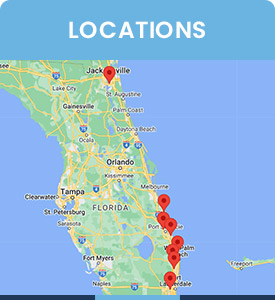
Dermatillomania, or skin-picking disorder, involves repetitive scratching or picking at one’s skin, often leading to damage and distress. At Psychiatry of the Palm Beaches, we offer comprehensive treatment, combining behavioral therapy and medication to help manage symptoms and improve overall well-being. For more information, contact us today or book an appointment online. Visit Psychiatry of the Palm Beaches serving Jacksonville, Boynton Beach, Palm Beach Gardens, Stuart, Royal Palm Beach, Port St. Lucie, Melbourne, Fort Lauderdale, and Jupiter, FL.


Table of Contents:
What is dermatillomania (skin-picking disorder)?
What causes dermatillomania?
What are the symptoms of dermatillomania?
How is dermatillomania diagnosed?
Dermatillomania (skin-picking disorder) is a behavioral condition that can interfere with daily life, causing both physical and emotional distress. While the behavior may be difficult to manage alone, seeking professional care is a key step toward recovery. At Psychiatry of the Palm Beaches, patients have the opportunity to access specialized treatments tailored to address the underlying factors driving the condition, offering effective strategies to regain control and improve overall well-being.
Dermatillomania is a disorder that is characterized by an uncontrollable urge to pick at one’s skin, often leading to physical damage such as lesions, scarring, or infections. The behavior can result from various causes including perceived imperfections on the skin, such as small blemishes or scabs, and is frequently linked to feelings of tension or anxiety, which are momentarily alleviated by the act of picking. While dermatillomania can significantly disrupt a person’s life, it is a treatable condition when approached with a combination of evidence-based therapies and a supportive care plan.
The causes of dermatillomania are highly varied, involving a combination of biological, psychological, and environmental factors. Neurological imbalances, particularly in serotonin levels, are believed to contribute to the compulsive nature of the disorder. Family history also plays a role, as individuals with close relatives experiencing obsessive-compulsive disorder (OCD) or similar conditions are at higher risk. Psychologically, dermatillomania is often linked to heightened levels of anxiety, stress, or depression, which can exacerbate the behavior. Environmental triggers, such as stressful life events or exposure to skin irritants, may also influence its onset or severity. Individuals with dermatillomania often experience significant emotional and social challenges due to the physical consequences of skin picking and the accompanying shame or guilt.
The condition may interfere with daily activities, relationships, and self-esteem, particularly when visible marks on the skin lead to self-consciousness. Despite these difficulties, treatment options such as cognitive-behavioral therapy (CBT) and, in some cases, medication, can help individuals gain control over their symptoms and improve their overall quality of life.
Dermatillomania arises from a variety of distinct causes but typically involves a combination of genetic, neurobiological, psychological, and environmental factors. Genetically, individuals with a family history of OCD or other anxiety-related disorders may have a predisposition to developing skin-picking behaviors. Neurobiological components, including serotonin imbalances, are also associated with the disorder, as these neurotransmitters play a key role in mood regulation and impulse control. Hormonal changes, particularly during puberty or hormonal fluctuations in adulthood, can further exacerbate symptoms in some individuals.
Psychological factors significantly contribute to the development and persistence of dermatillomania. The disorder is frequently linked to stress, anxiety, or trauma, with skin-picking behaviors serving as a maladaptive coping mechanism. Additionally, individuals with conditions like body dysmorphic disorder (BDD) or depression may be more susceptible, as these issues often amplify feelings of dissatisfaction with one’s appearance. The repetitive nature of the behavior is reinforced by temporary relief from emotional tension, creating a cycle that is difficult to break without intervention. Environmental elements, such as stressful life circumstances or exposure to specific triggers like skin irritants, can exacerbate the disorder or initiate episodes.
While these factors collectively contribute to the disorder, understanding their impact allows the specialists at Psychiatry of the Palm Beaches to establish targeted treatment plans. Therapeutic approaches often address both the underlying psychological causes and the habitual behaviors, helping individuals regain control and manage their symptoms effectively.
Dermatillomania is characterized by repeated skin-picking behaviors that result in noticeable physical harm. The most prominent symptom is the presence of lesions, scabs, or scars caused by frequent picking, often focused on areas such as the face, arms, or hands. These behaviors may occur in response to perceived imperfections or irregularities on the skin, even when no actual blemishes are present. Individuals may spend extended periods engaging in this activity, often losing track of time or becoming unaware of the severity of their actions.
The psychological impact of dermatillomania is significant, as individuals frequently experience feelings of shame, guilt, or frustration about their inability to control their behavior. Social withdrawal is common due to embarrassment about visible skin damage, further isolating individuals and contributing to feelings of loneliness or depression. These emotional challenges can perpetuate the cycle of skin picking, as stress and anxiety are known triggers for the behavior.
Other symptoms include repeated attempts to stop or reduce the behavior, often with little success, and a profound sense of distress or impairment in daily functioning. The condition may interfere with work, social relationships, and self-esteem, making professional intervention essential. Effective treatment often includes a combination of behavioral therapies, such as habit reversal training within CBT, and in some cases, medication to manage underlying anxiety or compulsive tendencies. By addressing both the physical and psychological aspects of the disorder, individuals can achieve significant improvements in their symptoms and overall well-being.
Diagnosing dermatillomania requires a thorough clinical evaluation to differentiate the condition from other medical or psychological issues. The process typically begins with an in-depth interview to assess the individual’s medical history as well as any history of skin-picking behaviors, including their frequency, intensity, and impact on daily life. Physical examinations are also conducted to identify signs of chronic picking, such as scabs, lesions, or scars, which often serve as visible markers of the disorder. To confirm a diagnosis, specialists at Psychiatry of the Palm Beaches will consider the diagnostic criteria outlined for excoriation disorder, which include recurrent skin picking that results in tissue damage, repeated attempts to stop or reduce the behavior, and significant distress or impairment in functioning. These criteria help ensure that the behavior is not better explained by another condition, such as a dermatological disorder or other psychiatric conditions like OCD or BDD. In some cases, standardized assessment tools may be used to measure the severity and impact of the disorder, providing a comprehensive understanding of the individual’s experiences. Once a diagnosis is established, treatment plans can be tailored to address both the behavioral and emotional aspects of the condition, promoting lasting recovery and improved quality of life.
Dermatillomania treatment is available at Psychiatry of the Palm Beaches. For more information, contact us today or book an appointment online. We serve patients from Boynton Beach FL, Delray Beach FL, Palm Beach Gardens FL, Jupiter FL, Stuart FL, Palm City FL, Royal Palm Beach FL, Wellington FL, Citrus Ridge FL, Jacksonville FL, Riverside FL, Port St. Lucie FL, Beau Rivage West FL, Melbourne FL, Palm Bay FL, Fort Lauderdale FL, Hollywood FL, Jupiter FL, North Palm Beach FL, and surrounding areas.
Check Out Our 5 Star Reviews



Additional Services You May Need
▸ Mental Wellness
▸ Relationship Coaching
▸ Depression and Mood Disorders
▸ Women’s Health
▸ Panic Disorder
▸ Medications Management
▸ Men’s Health
▸ Individual Psychotherapy
▸ Bipolar
▸ ADHD
▸ Geriatric Mental Health
▸ Couple’s Counseling
▸ Obsessive Compulsive Disorder
▸ Social Phobia Treatment
▸ Eating Disorders
▸ Post Traumatic Stress Disorder
▸ Psychotic Disorders